RUS ENG
Grant of the Government of the Russian Federation for the state support of scientific researches, which are conducted under the guidance of leading scientists in Russian educational institutions of higher professional education (agreement No. 11.G34.31.0065 dated October 19, 2011)

Regeneration of airways and lung
The official website of the project "Investigating the molecular mechanisms and underlying pathways of regenerative medicine approaches the tissue-engineering and cell therapy of airways and lungs"
| |
| |
Events and announcements | |
| |
| |
| |
| |
| |
| |
|
International Symposium and School of Young Scientists
“Prospects of regenerative medicine for tissue engineering of intrathoracic organs”
December 11, 2015, Kuban State Medical University, Krasnodar, Russia
International Symposium and School of Young Scientists
“Prospects of regenerative medicine for tissue engineering of intrathoracic organs”
(supported by the Grant of the Government of the Russian Federation designed for state support of research, conducted under the guidance of leading scientists in Russian educational institutions for higher professional education
(¹ 11.G34.31.0065)
09.00-09.15
Opening words: Sergey Alekseenko, chancellor, Kuban State Medical University
09.15-09.45
Paolo Macchiarini (Karolinska Institute; KSMU):
Megagrant Project Results 2011-2015
09.45-10.05
I. Ì. Spivak (Institute of Cytology, RAS)
Role of DNA repair mechanisms in the stem cells maintenance
10.05-10.25
Y.V. Parfyonova, P.I. Makarevich, K.V. Dergilev (Russian Cardiology Research and Production Complex):
Cell sheets technology for ischemic tissues regeneration.
10.25-10.45
R.V. Deev (Human Stem Cells Institute):
Gene-activated matrices technology for tissue engineering
10.45-11.05
T.E. Grigoriev (NRC “Kurchatov Institute”):
Porous materials for tissue engineering
11.05-11.15
E.À. Gubareva (KSMU):
Tissue-engineered diaphragm
11.15-11.30
E. V. Kuevda (KSMU):
Òissue-engineered lung
11.30-11.45
A. S. Sotnichenko (KSMU):
Tissue-engineered heart
11.45-12.00
I. V. Gilevich (KSMU, Krasnodar Regional Hospital ¹1):
Morpho-functional patterns of tissue-engineered tracheas transplantation in humans: Interim results of the NCT01997437 trial
12.00-12.15
I.S. Gumenyuk (KSMU): Image analysis and algorithm development, despite moderne regenerative medicine Lab
New diaphragms grown from stem cells offer hope of a cure for common birth defect and possibly future repairs of the heart
 An international collaboration between scientists in Sweden, Russia, and the United States has resulted in the successful engineering of new diaphragm tissue in rats using a mixture of stem cells and a 3D scaffold. When transplanted, it has regrown with the same complex mechanical properties of diaphragm muscle. The study is published in the journal Biomaterials, and offers hope of a cure for a common birth defect and possible future heart muscle repairs.
An international collaboration between scientists in Sweden, Russia, and the United States has resulted in the successful engineering of new diaphragm tissue in rats using a mixture of stem cells and a 3D scaffold. When transplanted, it has regrown with the same complex mechanical properties of diaphragm muscle. The study is published in the journal Biomaterials, and offers hope of a cure for a common birth defect and possible future heart muscle repairs.
The multidisciplinary team behind the current study includes world-renowned researchers in the field of regenerative medicine and tissue engineering; Paolo Macchiarini, MD, PhD, Director of the Advanced Center for Regenerative Medicine and senior scientist at Karolinska Institutet; Doris Taylor, PhD, Regenerative Medicine Research Director at the Texas Heart Institute; and Mark Holterman, MD, PhD, Professor of Surgery and Pediatrics at the University of Illinois College of Medicine in Peoria, working in collaboration with a research team at the Kuban State Medical University in Russia.
The diaphragm is a sheet of muscle that has to contract and relax constantly to allow breathing. It is also important in swallowing, and acts as a barrier between the chest cavity and the abdomen. Malformations or holes in the diaphragm are found in 1 in 2,500 babies and can cause extreme, often fatal, symptoms.
At the moment, surgical repair of large defects like these involves using an artificial patch, which will not grow with the infant and does not provide any contraction to assist with breathing. The new technique presented in Biomaterials could instead allow such replacements to be grown especially for babies from their own cells, which would provide all the function of diaphragm tissue and would grow with them.
The success of this study also offers hope for the possibility of regenerating heart tissue, which undergoes similar pressure as it contracts and relaxes with every beat.
“So far, attempts to grow and transplant such new tissues have been conducted in the relatively simple organs of the bladder, windpipe and esophagus. The diaphragm, with its need for constant muscle contraction and relaxation puts complex demands on any 3D scaffold; until now, no one knew whether it would be possible to engineer,” said Dr. Doris Taylor.
Dr. Paolo Macchiarini adds, "This bioengineered muscle tissue is a truly exciting step in our journey towards regenerating whole and complex organs. You can see the muscle contracting and doing its job as well as any naturally-grown tissue - there can be no argument that these replacements are truly regenerated, and the possibilities that this opens up for the future are enormous."
The field of tissue engineering involves 'growing' new tissues or organs from stem cells on three dimensional 'scaffolds,' which give both structural support and shape to the new tissue and guide the differentiation and proliferation of the stem cells. Engineered new tissues can not only help patients avoid the need for an organ donation, but also the need for the recipient to take immunosuppressant drugs.
In the current study, the researchers took diaphragm tissue from donor rats and removed all the living cells from it using a series of chemical treatments. This process removes anything that might cause an immune response in the recipient animals, while keeping all the connective tissue – or extracellular matrix – which gives tissues their structure and mechanical properties. When tested in vitro, these diaphragm scaffolds at first appeared to have lost their important rubber-like ability to be continually stretched and contracted for long periods of time. However, once seeded with bone marrow derived alloegenic stem cells and then transplanted into the animals, the diaphragm scaffolds began to function as well as undamaged organs.
The method must now be tested on larger animals before it can be tried in humans, but the hope is that tissue-engineered repairs for congenital diaphragm malformations will be at least as effective as current surgical options with the added benefit of growing with children throughout their lives.
The study was supported and financed by Bioengineering of Tracheal Tissue and the Government of the Russian Federation Grant.
Publication: ‘Orthotopic transplantation of a tissue engineered diaphragm in rats’, Elena A. Gubareva, Sebastian Sjöqvist, Irina V. Gilevich, Alexander S. Sotnichenko, Elena V. Kuevda, Mei Ling Lim, Neus Feliu, Greg Lemon, Konstantin A. Danilenko, Ramazan Z. Nakokhov, Ivan S. Gumenyuk, Timofei E. Grigoriev, Sergey V. Krasheninnikov, Alexander G. Pokhotko, Alexander A. Basov, Stepan S. Dzhimak, Ylva Gustafsson, Geoanna Bautista, Antonio Beltrán Rodríguez, Vladimir M. Pokrovsky, Philipp Jungebluth, Sergei N. Chvalun, Mark J. Holterman, Doris A. Taylor and Paolo Macchiarini, Biomaterials, online XX November 2015. doi:10.1016/j.biomaterials.2015.11.020
For further information, please contact:
Paolo Macchiarini, MD, PhD,
Karolinska Institutet
Tel: +46 76-050 32 13
E-mail: paolo.macchiarini@ki.se
Press Office Karolinska Institutet
About the universities:
Kuban State Medical University
Karolinska Institutet
Texas Heart® Institute
University of Illinois College of Medicine in Peoria (UICOMP)
Poster Award Nominee
 Poster presentation “Tissue engineered lungs in rats and nonhuman primates” by Elena Kuevda, PhD, International Center of Regenerative Medicine KubGMU, was nominated for the Poster Award at the World Conference on Regenerative Medicine (Leipzig, October 21-23, 2015). It was selected among 20 other posters from 282 presented at the conference.
Poster presentation “Tissue engineered lungs in rats and nonhuman primates” by Elena Kuevda, PhD, International Center of Regenerative Medicine KubGMU, was nominated for the Poster Award at the World Conference on Regenerative Medicine (Leipzig, October 21-23, 2015). It was selected among 20 other posters from 282 presented at the conference.
Congratulations!!
Presentation of “Megagrant”

Presentation of “Megagrant” – a documentary novel by Elena Kokurina, was held in the Oval hall of Rudomino All-Russia State Library for Foreign Literature on May 28.
The main character, professor Paolo Macchiarini, won the grant of Russian Federation for research on regeneration of organs and tissues, including transplantations of organs created by his unique method.
This novel tells a fascinating and dramatic story of a foreign scientist who faced a great number of problems and surprises, experienced success and disappointment, and finally learnt to survive and live in Russia. Everyday life of the Russian laboratory is shown on a background of development of the world regenerative medicine. Does the main character of the novel hurry over translating new technologies into clinic even if a human life depends on it? What happened to his first patients? Will he manage to achieve his main goal – creation of a heart – in conditions of Russian reality?
The novel was published by a publishing house “Boslen” and is the first novel from the new series “The pulse of time”. The story is happening here and now, and no one knows what the ending will be like, as well as in our life.
Alongside with the author and publishers the characters of the novel also took part in the presentation – all the people, who joined hands working under this project during these years and formed a strong team of scientists from different fields of science:
Paolo Macchiarini, professor of regenerative surgery, Karolinska Institute (Sweden),
Andrey Redko, professor, vice-chancellor of the Kuban state medical university,
Vladimir Parshin, professor, head of the thoracic surgery department of the 1st Moscow state medical university hospital,
Roman Deev, candidate of medical science, Research director of the Human stem cells institute, science editor of the novel,
Irma Sakhuria, candidate of biological science, director general of “Chembio”,
Timofey Grigoriev, candidate of physical-mathematical science, deputy head of the polymer materials laboratory RC “Kurchatov Institute”.
There were also many other guests – researchers, writers and journalists.
The ministry of education and science of the Russian Federation was represented by the head of Science and technology department S. V. Salikhov. He underlined the importance of popularization of “megagrant program”, especially if it is done in such an unusual way as a documentary novel.
Megagrant is a documentary novel by Elena Kokurina, issued by the publishing house Boslen
The author is a science journalist and a member of the Russian Association of Science Writers and Journalists, having worked on the newspapers Obstchaya gazeta and Moskovskie novosti, and magazines Russki Newsweek and V mire nauki. Her book tells a story in which she herself played a direct part.
The main character of the novel is famous surgeon and specialist in the field of regenerative medicine Paolo Macchiarini. He was one of the winners of the so-called 'megagrant competition' in 2011, receiving a Grant of the Government of the Russian Federation to create a high-end research laboratory in Krasnodar, Russia.
The book, which is based on fact, tells the fascinating and dramatic story of a foreign scientist who faces a great number of problems and surprises, experiences success and disappointment, and finally learns to survive and live in Russia.
Here he finds reliable partners in the form of the great surgeons of Krasnodar regional hospital ¹1, and the employees of the Kuban state medical university. Everyday life of the Russian laboratory is shown at a background of the development of the new science of regenerative medicine in the world.
The novel Megagrant - which is the first of a new series called The Pulse of Time from the publishing house Boslen – is a history, made today...now, and in which the reader has a unique opportunity to take part. The unpredictable plot of a real life makes it captivating from the very first pages: there is nothing that one can change or correct as it unfolds. No one can stop “the pulse of time”.
International Symposium “Regeneration of intrathoracic organs and tissues” conducted in KSMU

It is already the fourth symposium conducted within the Grant ofthe Government of the Russian Federation. As usual,it included the School of young scientists. More than 400 people from the different cities of Russia took part in it this time.
The presentations were divided into two sections – plenary and research. In the frames of the first section within the School of young scientists the invited speakers spoke about fundamental aspects of regenerative medicine. In particular, - about the cellular mechanisms resistant to regeneration, features of celltherapy, properties of polymeric materials at their interaction with living cells. Presentations were submitted by our long-termcollaborators from the Institute of cytology of the Russian Academy of Sciences (V. M.Mikhelson - I. M. Spivak), Research Center Kurchatov Institute (S. N. Chvalun), and also - Federal State Budgetary Institution Russian Cardiology Research-and-Production Complex of the Ministry of Healthcare of Russia and Faculty of fundamental medicine of MSU. Professor Elena Parfyonova told about transplantation of heart resident stem cells in the form of multilayered cell layers at an experimental myocardial infarction.
Traditionally the leading scientist, Professor Paolo Macchiarini,presented the final report on the results obtained in the course of implementation of the project and plans for the next year which are mostly focused on the development of the tissue-engineered heart, lungs and diaphragm on models of the non-human primates.
The foundation was laid in 2014, what was reportedby the members of the research team Elena Gubareva, Elena Kuevda, Alexander Sotnichenko and Irina Gilevich. Their presentations provoked strong interest in participants and guests.
International Symposium and School of Young Scientists
“Regeneration of intrathoracic organs and tissues” (in support of the Grant of the Government of Russian Federation ¹ 11.G34.31.0065)
December 19, 2014, Kuban State Medical University, Krasnodar, Russia
9.00-12.45
Opening words:
Sergey Alekseenko, chancellor, Kuban State Medical University
Keynote lectures (20 min):
Victor Mikhelson (Institute of Cytology RAS, St.Peterburg) Cell mechanisms standing against regeneration
Elena Parfyonova (Russian National Heart Center, Moscow) Multilayered resident cardiac stem cell sheets for myocardial infarction repair
Sergey Chvalun (Kurchatov Center, Moscow) Rubber elasticity of collagen networks
Paolo Macchiarini (Karolinska Institute, Sweden, Kuban State Medical University, Krasnodar) Lessons learned from the Megagrant Project
Investigation reports (15 min):
Elena Gubareva – Kuban State Medical University (Krasnodar) Tissue engineering diaphragm in rats and NHP models
Alexander Sotnichenko - Kuban State Medical University (Krasnodar) Tissue engineering heart
Elena Kuevda - Kuban State Medical University (Krasnodar) Tissue engineering lung
Irina Gilevich – Krasnodar Regional Hospital ¹1, Kuban State Medical University (Krasnodar) Clinical stem cell mobilization
12.45-14.00 - lunch
The Gold Medal for the heart
 Alexander Sotnichenko, post-graduate student of pathological anatomy department, the governmental grant researcher, was awarded the Gold medal “All-Russia Exhibition Center Laureate” on the XIV All-Russia exhibition of research and technological achievements of the young scientists. The exhibition was conducted in All-Russia Exhibition Center in Moscow on June 24-27, 2014.
Alexander Sotnichenko, post-graduate student of pathological anatomy department, the governmental grant researcher, was awarded the Gold medal “All-Russia Exhibition Center Laureate” on the XIV All-Russia exhibition of research and technological achievements of the young scientists. The exhibition was conducted in All-Russia Exhibition Center in Moscow on June 24-27, 2014.
Alexander made a presentation of his project “Experimental tissue engineering of rat heart” which is implemented in the frames of the government of the Russian Federation at the International research, clinical and educational center of regenerative medicine of KSMU.
 Total amount of participants of this competition was 650. These authors of research and technological projects aged up to 30 years came from different parts of Russia, near- and far-abroad countries. The VI International research-to-practice conference “Research and technological achievements of the young scientists is the way to the knowledge-based society” was also carried out in All-Russia Exhibition Center under the support of the Ministry of education and science of the Russian Federation.
Total amount of participants of this competition was 650. These authors of research and technological projects aged up to 30 years came from different parts of Russia, near- and far-abroad countries. The VI International research-to-practice conference “Research and technological achievements of the young scientists is the way to the knowledge-based society” was also carried out in All-Russia Exhibition Center under the support of the Ministry of education and science of the Russian Federation.
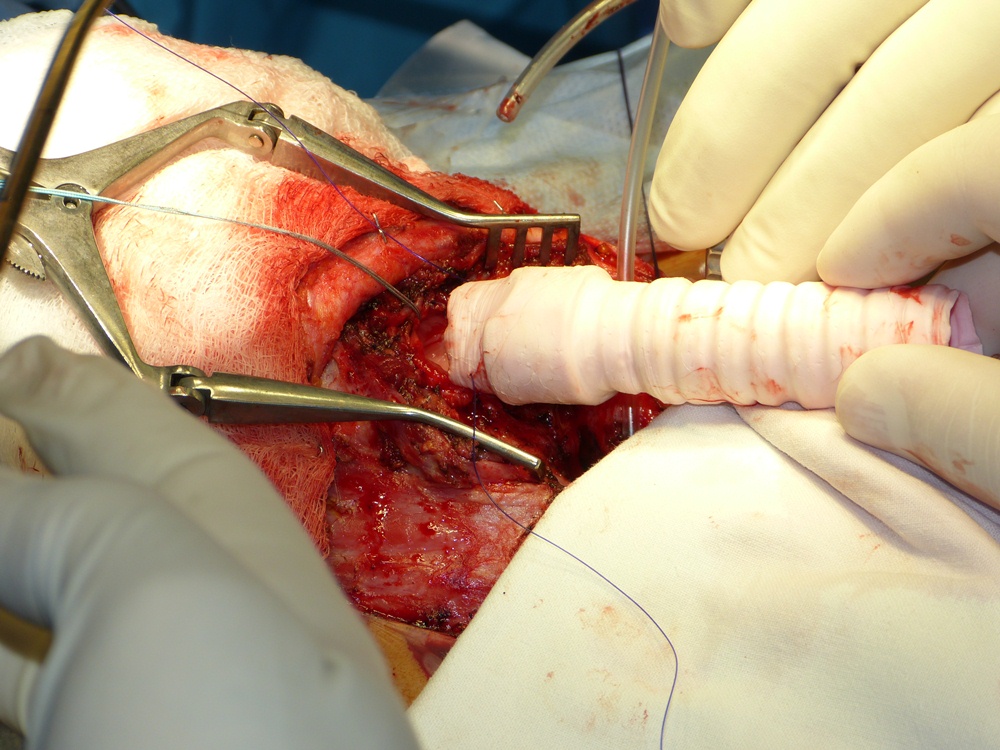
Transplantation of tissue-engineered has been carried out in Krasnodar
 June 3, 2014: A patient from Crimea underwent tissue-engineered tracheal transplantation in Krasnodar regional clinical hospital ¹1. Seven years ago the young man was injured in a car accident and since that time underwent 14 surgeries in Ukraine, including Kiev. However, no improvement has been observed.
June 3, 2014: A patient from Crimea underwent tissue-engineered tracheal transplantation in Krasnodar regional clinical hospital ¹1. Seven years ago the young man was injured in a car accident and since that time underwent 14 surgeries in Ukraine, including Kiev. However, no improvement has been observed.
The transplantation was carried out by the regenerative medicine professor of Karolinska Institute Paolo Macchiarini, the head doctor of the Krasnodar regional clinical hospital ¹1 Professor Vladimir Porkhanov. The surgery lasted about 6 hours. The patient feels well; he can speak and breathe normally.
Trachea preparation process was performed in RCH ¹1, in a clinical laboratory of the International research, clinical and educational center of regenerative medicine by the Megagrant research team.
Tissue engineering has been used to construct natural oesophagi, which in combination with bone marrow stem cells have been safely and effectively transplanted in rats
 Alexander Sotnichenko, 26, PhD student of the Kuban State Medical University (Krasnodar, Russia) took part in this study. For the first time Russian researcher becomes co-author in the publication for Nature Com.
Alexander Sotnichenko, 26, PhD student of the Kuban State Medical University (Krasnodar, Russia) took part in this study. For the first time Russian researcher becomes co-author in the publication for Nature Com.
The new method has been developed by researchers at KarolinskaInstitutet in Sweden, within an international collaboration lead by Professor Paolo Macchiarini. The technique to grow human tissues and organs, so called tissue engineering, has been employed so far to produce urinary bladder, trachea and blood vessels, which have also been used clinically. However, despite several attempts, it has been proven difficult to grow tissue to replace a damaged oesophagus.
In this new study, the researchers created the bioengineered organs by using oesophagi from rats and removing all the cells. With the cells gone, a scaffold remains in which the structure as well as mechanical and chemical properties of the organ are preserved. The produced scaffolds were then reseeded with cells from the bone marrow. The adhering cells have low immunogenicity which minimizes the risk of immune reaction and graft rejection and also eliminates the need for immunosuppressive drugs. The cells adhered to the biological scaffold and started to show organ-specific characteristics within three weeks.
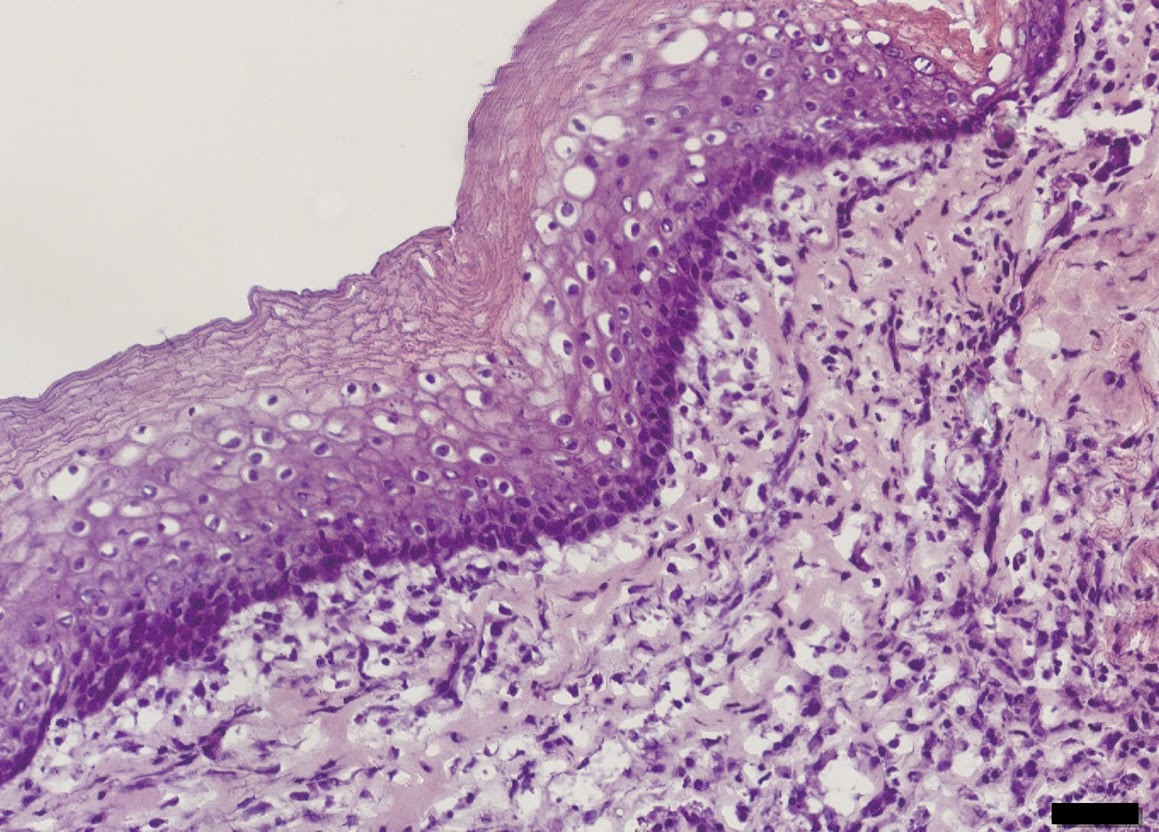 The cultured tissues were used to replace segments of the oesophagus in rats. All rats survived and after two weeks the researchers found indications of the major components in the regenerated graft: epithelium, muscle cells, blood vessels and nerves.
The cultured tissues were used to replace segments of the oesophagus in rats. All rats survived and after two weeks the researchers found indications of the major components in the regenerated graft: epithelium, muscle cells, blood vessels and nerves.
“We believe that these very promising findings represent major advances towards the clinical translation of tissue engineered esophagi”, says Paolo Macchiarini, Director of Advanced center for translational regenerative medicine (ACTREM) at KarolinskaInstitutet.
Tissue engineered organs could improve survival and quality of life for the hundreds of thousands of patients yearly diagnosed with oesophageal disorders such as cancer, congenital anomalies or trauma. Today the patients’ own intestine or stomach is used for esophageal replacements, but satisfactory function rarely achieved. Cultured tissue might eliminate this current need and likely improve surgery-related mortality, morbidity and functional outcome.
http://www.nature.com/ncomms/2014/140415/ncomms4562/full/ncomms4562.html
 For further information, please contact:
For further information, please contact:
Professor Paolo Macchiarini, MD, PhD
Advanced Center for Translational Regenerative Medicine (ACTREM)
Department of Clinical Science Intervention and Technology (CLINTEC), KarolinskaInstitutet
Telephone: +46 760503213
Email: paolo.macchiarini@ki.se
For fhotos and videos follow this llink:
https://drive.google.com/folderview?id=0B5JFQA7zPvtVeGlzUFBRMEJkQlk&usp=sharing
Grant Council of the Russian Government made decision on the Project’ extension
Based on the results of international assessment of the results of 2011-2013 and application, submitted by the PI and the Kuban state medical university, Grant Board adopted a resolution of expediency of 2 years prolongation of the project conducted, financed from the Federal budget in amount of 22,5 million rubles in 2014, the amount of co-financing attracted by the University for research is unlimited. Amount of co-financing, attracted by the University for research in 2015, must be not less than 22,5 million rubles. More info.
December 11, 2013: International Symposium and the 4thRegenerative Medicine School for Young Scientists “Organs and Tissues Regeneration” was conducted on the basis of the International Research, Clinical and Educational Center of Regenerative Medicine
 Professor Doris Taylor, Regenerative Medicine Research Director of the Texas Heart Institute (USA, Texas), delivered a keynote lecture.
Professor Doris Taylor, Regenerative Medicine Research Director of the Texas Heart Institute (USA, Texas), delivered a keynote lecture.
Doris Taylor is regarded as the heart regeneration pioneer. Together with her collaborators, she managed to perform “complete decellularization” of lab animal and human hearts. Then the scaffold re-seed with stem cells partially acquired the properties and functional parameters of a regenerated beating heart. That is the first visit of Doris Taylor to Russia. Her lecture is called “Engineering human lung and heart tissues”.
The reporters include Professor of Karolinska Institute and Kuban State Medical University Paolo Macchiarini. His presentation is devoted to the progress of airway regeneration project implemented in the frames of Megagrant and plans for the next two years.
The other speakers are: Professor Sergey Chvalun, Head of the Polymer Materials Laboratory of the Kurchatov Institute; Professor Sergey Orlov, Director of the Medical Primatology Research Institute of the Russian Academy of Medical Sciences; Professor Vladimir Porkhanov, Associate Member of the Russian Academy of Medical Sciences, Head Physician of Regional clinical hospital No.1; and David Green, CEO, Harvard Apparatus Regenerative Technology (Holliston, USA).
A foreign patient underwent trachea transplantation in Krasnodar
 A 42-year-old patient from Jordanian, who underwent a unique tracheal transplantation performed with the use of bioengineered scaffold seeded with patient’s own cells, was dismissed from Krasnodar regional clinical hospital ¹1. According to Hospital press-office, postoperative care lasted for about a month; the patient is doing well now.
A 42-year-old patient from Jordanian, who underwent a unique tracheal transplantation performed with the use of bioengineered scaffold seeded with patient’s own cells, was dismissed from Krasnodar regional clinical hospital ¹1. According to Hospital press-office, postoperative care lasted for about a month; the patient is doing well now.
The transplantation was carried out on August 9, 2013 by the regenerative medicine professor of Karolinska Institute (Sweden), the leading scientist of the governmental Megagrant Paolo Macchiarini, the head doctor of the RCH ¹1, corresponding member of RAMS, Professor Vladimir Porkhanov and his deputy, thoracic surgeon, candidate of medical science Igor Polyakov together with other members of surgical team.
Almost 20 years passed from the day when Hanaan S., the patient, was badly injured in a car accident. Long-term artificial lung ventilation caused a tracheal stenosis. He had breathing difficulties and wasn’t able to move and talk. He underwent a number of surgeries, having just a temporary effect, and as time passed the tracheal lumen grew smaller. He was afraid to fall asleep, since he suffered from sleep apnea caused by the collapse of softened trachea. As a doctor, Hanaan kept trying to find some information on more effective technologies that could help him. In 2006 he was examined in Boston (USA), however he was denied a surgery, his case was considered too difficult (it is believed that there is no chance to help a patient when such a large patch of trachea is damaged). At last he revealed about professor Macchiarini’s method and the fact that regenerative medicine technologies grow rapidly in Krasnodar and two artificial trachea transplantations with the use of patients’ own cells were performed in summer 2012. By that time Paolo Macchiarini had performed 6 transplantations of this kind in the frames of international clinical trial all over the world.
Hanaan’s surgery was difficult and lasted for more than 6 hours. “I had no doubt that everything will be fine”, - said the patient, who was able to breathe and speak normally almost immediately after anesthesia recovery.
Process was the same as that of the previous surgeries: 48 hours before the transplantation mononuclear cells were isolated from patient’s bone marrow sample by means of special equipment. An artificial scaffold was seeded with these cells and then it was placed into a bioreactor, where cell proliferation and adhesion occurred. In 48 hours the scaffold is ready to be transplanted.
“However the technology is a little bit changed and refined each time – that is the essence of translational medicine, - says professor Macchiarini. In this particular case our partners from the USA and Germany improved the composition of the scaffold and the bioreactor based on previous experience. The entire scaffold seeding was performed by the specialists from Krasnodar Hospital, who were trained in Karolinska Institute last year, without exterior help at their own laboratory. And they did it excellent!”
It is planned to continue conduction of surgeries, the next transplantations are planned for the nearest future.
Trachea transplant at Children's Hospital of Illinois gives korean toddler new windpipe

Child is first in the world to receive tissue-engineered bioartificial trachea
grown with her own cells.
(Peoria, IL USA / April 30, 2013) – In a pioneering, first of its kind in the world operation, an international team of surgeons at Children's Hospital of Illinois created and transplanted a windpipe into a 32-month-old Korean toddler born with a rare, fatal, congenital abnormality in which her trachea failed to develop.
During the revolutionary operation, the surgical team implanted a tissue engineered stem cell based artificial windpipe in Hannah Warren, who had spent her entire life living in a neonatal intensive care unit in a hospital in Seoul, South Korea. Unable to breathe, talk, swallow, eat or drink on her own since birth, Hannah would have died without a trachea transplant.
The groundbreaking, nine hour operation took place at Children’s Hospital of Illinois, part of OSF Saint Francis Medical Center, in Peoria, Illinois, on April 9, 2013. It is the first time a child has received a tissue-engineered, bioartificial trachea, which was made using non-absorbable nanofibers and stem cells from her own bone marrow. Because no donor organ was used, the remarkable procedure virtually eliminates the chance of her immune system rejecting the transplant.
It is expected that in the coming months, she will be able to return home with her family and lead a normal life.
“The most amazing thing, which for a little girl is a miracle, is that this transplant has not only saved her life, but it will eventually enable her to eat, drink and swallow, even talk, just like any other normal child,” said Dr. Paolo Macchiarini, Professor of Regenerative Surgery at the Karolinska Institutet, Stockholm, Sweden and lead surgeon in the case. “She will go from being a virtual prisoner in a hospital bed to running around and playing with her sister and enjoying a normal life, which is a beautiful thing.”

Hannah arrived in Peoria in March accompanied by a medical team and her family: father Darryl, who is Canadian, mother Young-Mi who is Korean, and 4-year-old-sister, Dana.
“All we have ever wanted since Hannah was born was to be able to bring her home and be a regular family. Hannah has been through so much and defied the odds. She is our little miracle,” said Darryl Warren. “Words cannot express our thanks to everyone who has helped make this dream a reality. We know one day soon we will get to make that trip home.”
“It has been a privilege to be a part of this life-changing moment for Hannah and to provide care for her and her family. She embodies what we do for all those who come to us in need and truly allows us to live the Sisters’ Mission,” said Margaret Gustafson, President of Children’s Hospital of Illinois. “Hannah continues her recovery, cared for by a team including pulmonologists, hematologists, intensivists, nurses, respiratory therapists; physical, occupational and speech therapists, and supportive services.”
For the physicians in this case, and the staff at Children's Hospital of Illinois and OSF Saint Francis Medical Center, this history making procedure is an exciting, promising advancement in the field of regenerative medicine.
“Hannah’s case is a great example of how the international community can work together to save a child’s life”, said Dr. Mark Holterman, Professor of Surgery and Pediatrics at University of Illinois College of Medicine at Peoria (UICOMP) and co-surgeon of the case.
“We are humbled to have been a part of this amazing effort. Advanced pediatric patient care and scientific investigation are at the heart of our work here in Peoria. Hannah is an amazing young girl and our work with her will no doubt go a long way in helping others in the years to come, not only in Peoria but in the United States,” said Dr. Richard Pearl, Surgeon-in-Chief at Children’s Hospital and Professor of Surgery and Pediatrics at UICOMP.

Added Dr. Macchiarini: “The ultimate potential of this stem-cell based therapy is to avoid human donation and life-long immune suppression and to be able to replace complex tissues, and sooner or later, whole organs, with totally artificial lab-made scaffolds and autologous stem cells. We are crossing frontiers with these transplants."
In addition to members of Hannah’s surgical team and staff of clinical caregivers, the following provided invaluable support for the success of this groundbreaking surgery:
Advanced Center for Translational Regenerative Medicine, Karolinska Institutet, Stockholm, Sweden: Provided pre-clinical and scientific evidence for the stem-cell based technology
Russian Megagrant Project "Regeneration of airways and lung" (¹ 11.G34.31.0065), Krasnodar, Russia: The young specialists at the Kuban State Medical University contributed to the translational science of Hannah’s transplantation.
ABOUT CHILDREN’S HOSPITAL OF ILLINOIS:
Children's Hospital of Illinois is the third largest pediatric hospital in Illinois and the only full service tertiary hospital for kids downstate. With 124 beds and more than 115 pediatric subspecialists, Children's Hospital cares for more children in Illinois than any hospital outside of Chicago. Formally established as a pediatric hospital within the walls of OSF Saint Francis Medical Center in 1990, Children's Hospital has over 5,000 admissions; 2,200 newborn deliveries, and 18,000 emergency department visits each year. http://www.childrenshospitalofillinois.org/
ABOUT OSF SAINT FRANCIS MEDICAL CENTER:
OSF Saint Francis Medical Center, with 616 beds and more than 900 physicians, is the fourth-largest medical center in Illinois. A major teaching affiliate of the University of Illinois College of Medicine at Peoria, it is the area’s only Level I Trauma Center, the highest level designated in trauma care. It serves as the resource hospital for emergency medical services for north-central Illinois. It is home to Children’s Hospital of Illinois and the Illinois Neurological Institute. OSF Saint Francis and Children’s Hospital have been designated Magnet Status for excellence in nursing care since 2004. http://osfsaintfrancis.org/
First Heart - Lung Decelluarization in Russia
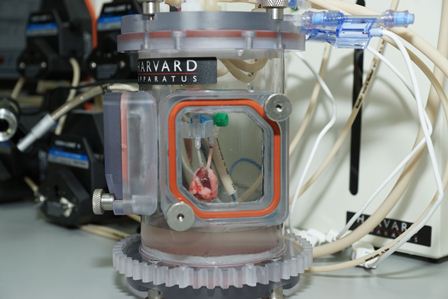 The novel equipment ORCA (Organ Regeneration Collection Analysis) Bioreactor - system specially designed to meet the needs of the regenerative medicine – was installed and started up in the Center of Regenerative Medicine of Kuban state medical university. The system is able to address the needs of both the decellularization (total cell removal) and recellularization (seeding with living cells) processes of various organs. As amatter of fact this system allows creation of a new organ. Bioreactors installation is a platform for development and introduction of new regenerative technologies, new direction of global medicine development.
The novel equipment ORCA (Organ Regeneration Collection Analysis) Bioreactor - system specially designed to meet the needs of the regenerative medicine – was installed and started up in the Center of Regenerative Medicine of Kuban state medical university. The system is able to address the needs of both the decellularization (total cell removal) and recellularization (seeding with living cells) processes of various organs. As amatter of fact this system allows creation of a new organ. Bioreactors installation is a platform for development and introduction of new regenerative technologies, new direction of global medicine development.
The system was purchased in the frames of the Megagrant of the Government of the Russian Federation. This grant was won by the University together with regenerative surgery Professor of Karolinska Institute, Stockholm, Paolo Macchiarini. Two unique tracheal transplantations were performed at the Regional clinical hospital N1; the tracheas for these transplantations were created with the use of nanocomposite artificial scaffold seeded with the patient’s cells.
Research starting at the Center of regenerative medicine of Kuban state medical university now opens up the possibilities for creation not only trachea, but other vital organs as well such as heart and lung in the future.
 There are two types of bioreactors installed in Krasnodar – for work with isolated organs of small and large animals, which are equipped with special cameras for heart, lungs, esophagus and trachea. Physiological conditions can be mimicked through control algorithms that regulate flow rates, profiles, and pressures.
There are two types of bioreactors installed in Krasnodar – for work with isolated organs of small and large animals, which are equipped with special cameras for heart, lungs, esophagus and trachea. Physiological conditions can be mimicked through control algorithms that regulate flow rates, profiles, and pressures.
At the present moment only 12 laboratories all over the world are equipped with facilities of this kind. 10 of them are located in USA and only 2 are in Europe – at Karolinska Institute, Sweden, and at Kuban state medical university, Russia.
Harvard Apparatus company specialists – producers of the equipment - started to train the specialists from the Center of regenerative medicine of KSMU to work with the “life reactors”.
 Cooperation with the researchers from Harvard is the small part of the vast collaboration, built in the frames of the project. It includes a number of Russian and foreign scientific and medical centers operating in various fields of science. Recently there were reached two agreements with Research institute of medical primatology RAMS and polymer materials laboratory RDE “Kurchatov Institute”.
Cooperation with the researchers from Harvard is the small part of the vast collaboration, built in the frames of the project. It includes a number of Russian and foreign scientific and medical centers operating in various fields of science. Recently there were reached two agreements with Research institute of medical primatology RAMS and polymer materials laboratory RDE “Kurchatov Institute”.
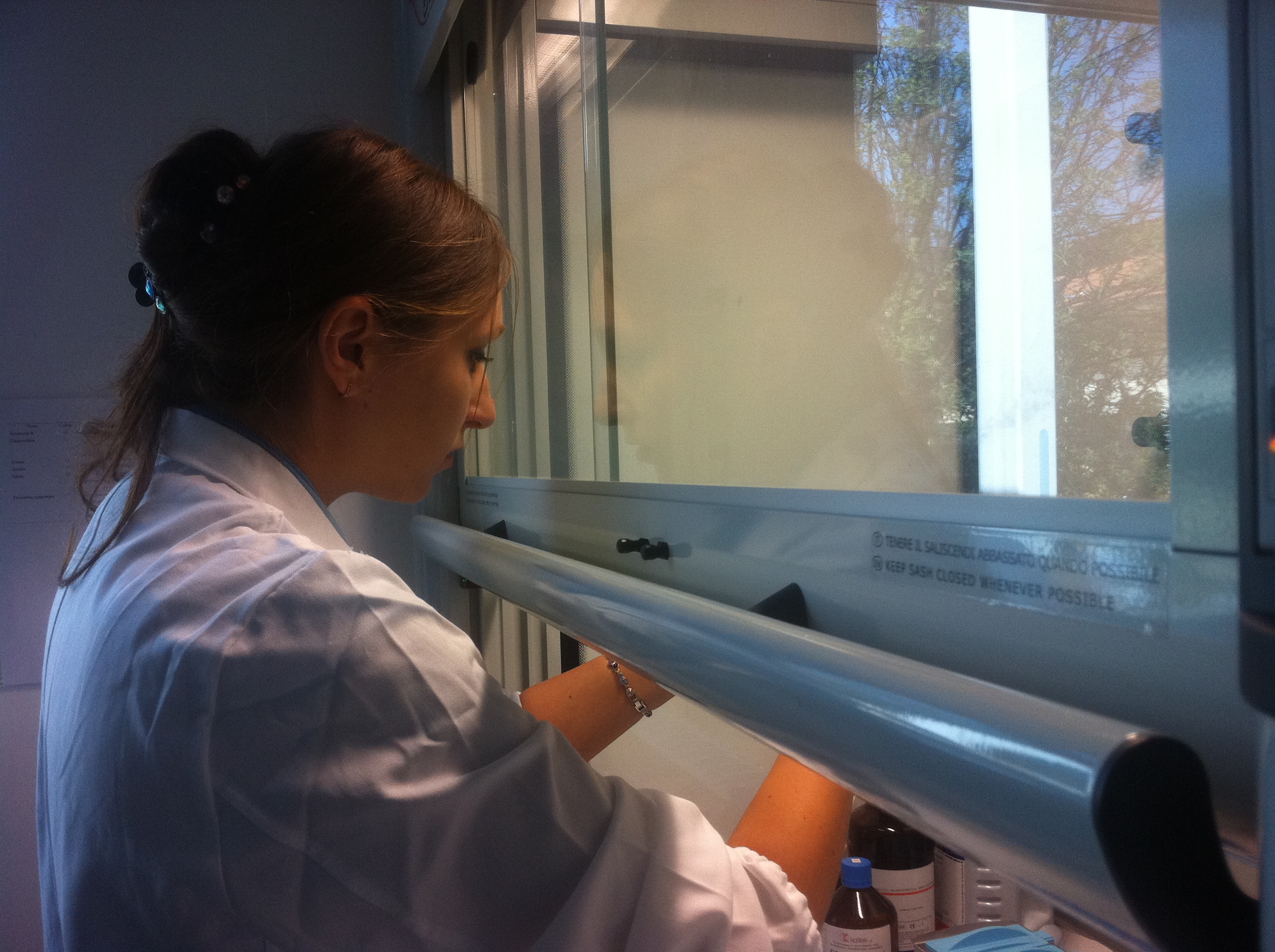
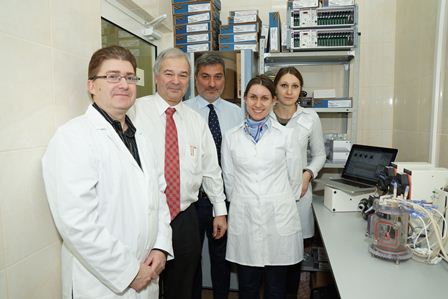
Center of Regenerative Medicine is opened in Krasnodar
 Professor Macchiarini and young scientists demonstrated the equipment, acquired in the frames of the grant of the Government of the Russian Federation, and told the guests about the research that will be carried out in the new laboratory. That is a wide range of works on regeneration mechanisms investigation, tissue-engineered transplants and bioengineered organs creation. The University’s basic research laboratory will be in a close connection with the clinical laboratory, based in the Regional clinical hospital ¹1. This provides the possibility to implement translational research in the following way: laboratory – clinic – laboratory.
Professor Macchiarini and young scientists demonstrated the equipment, acquired in the frames of the grant of the Government of the Russian Federation, and told the guests about the research that will be carried out in the new laboratory. That is a wide range of works on regeneration mechanisms investigation, tissue-engineered transplants and bioengineered organs creation. The University’s basic research laboratory will be in a close connection with the clinical laboratory, based in the Regional clinical hospital ¹1. This provides the possibility to implement translational research in the following way: laboratory – clinic – laboratory.
The center of regenerative medicine of KSMU was built and equipped in unbelievably short terms – it took less than a year. Today this laboratory is one of the best not only in Russia, but in Europe as well. “Even my laboratory at Karolinska Institute is worse in a number of respects”, - said Professor Macchiarini to the journalists.
 However, the state-of-the-art equipment is the first stage, it is still needed to bring life into the laboratory, and this kind of equipment requires high-qualified specialists. This was one of the points of the III All-Russian School for young scientists «Global experience of heart and lungs bioengineering», which was carried out at the University on November 8. The young scientists, participants of the grant who had been trained at the leading Russian and European centers, presented their first scientific papers. Roman Deev – medical director of the Human Stem Cells Institute and executive editor of the journal “Cell transplantology and tissue engineering” (Moscow) – shared the experience of cell technology training of the young specialists from KSMU.
However, the state-of-the-art equipment is the first stage, it is still needed to bring life into the laboratory, and this kind of equipment requires high-qualified specialists. This was one of the points of the III All-Russian School for young scientists «Global experience of heart and lungs bioengineering», which was carried out at the University on November 8. The young scientists, participants of the grant who had been trained at the leading Russian and European centers, presented their first scientific papers. Roman Deev – medical director of the Human Stem Cells Institute and executive editor of the journal “Cell transplantology and tissue engineering” (Moscow) – shared the experience of cell technology training of the young specialists from KSMU.
The grant leading scientist, Professor Paolo Macchiarini presented his lecture “Bioengineering intrathoracic organs and tissues”, in which he stated his views on regenerative medicine development prospects in the world and in Russia.
Video:
3rd School for young scientists with international participation “Global experience of heart and lungs bioengineering” , November 8, 2012
November 8, 2012
Kuban State Medical University
Krasnodar, Russia
At the Karolinska Institute in Sweden, rat hearts and lungs are washed of living cells to reveal the extracellular structure
At the Karolinska Institute in Sweden, rat hearts and lungs are washed of living cells to reveal the extracellular structure. This photo opens the article in the New York Times (16/09/2012) "Organ Tailor-Made With Body's Own Cells", devoted to the work and ideas of Professor Paolo Macchiarini and his lab.
Full text
Online questions to Professor Macchiarini
 Alexander B. (Moscow)
Alexander B. (Moscow)
Who first proposed the method of artificial (tissue-engineering) trachea? Does the implementation of this idea belong to you?
There have been several attempts to replace the trachea with artificial prosthesis in the 70’. By that time, no cells were seeded on the prostheses and the outcome was about a mortality rate of percent due to infection, dislocation, granuloma formation, mediastinatis, etc. We were the first group that combined all the classical components of tissue engineering organ and tissue replacements, namely the scaffolds, cells and bioreactor in the preclinical and clinical scenario.
Gimat D. (Makhachkala)
What conditions do you consider to be "ideal" (i.e, the so-called "ideal model") for the cultivation of cells in the graft, and what conditions - the real (within the capabilities of existing technologies), and what - are implemented within your practice and work?
Based on our previous studies, the ideal culture condition for a tubular structure like the trachea is a continuous rotation of the scaffold passing via both, a gas and liquid phase; We developed this method together with the Technical University of Milano, Italy (Prof. Mantero and Drs. Asnaghi). It is very important to combine the expertise and knowledge of both cellular biologists and engineers, and many others
Read more
The patients were discharged after first bioartificial stem-cell based laryngo-tracheal transplantation
Two patients were discharged from Krasnodar Clinical Hospital on the 14th of July, 2012, after successful first bioartificial stem-cell based laryngo-tracheal transplantation performed by Paolo Macchiarini, Professor of Regenerative Medicine of Karolinska Institute (Sweden) and Vladimir Porhanov, head of oncological and thoracic department of Kuban State Medical University (Russia).
Julia Tuulik, 33 years old mother of one child from Saint-Petersburg, and Alexander Zozulya, 28, from Rostov Region, both suffered from a narrowing of the laryngo-tracheal junction for which they already had a failed previous surgeries. Both are the victims of motorcar accidents more then 2 years ago. Transplantation was the last resource for the patients to breath and speak normally and get a normal quality of life. Immediately after transplantation they were able to speak and breath. Now, 3 weeks after, they recovered completely.
Lab tests (flow cytometry) shows the increased level of circulating progenitor cells. Progenitor cells were mobilized with pharmacological intervention to boost the generation of the
implanted grafts. There was also observed (cytology) the appearance of metaplasm epithelium in the anastomosis.
“These are the best results, I‘ve got so far after 15 transplantations using donor’s and artificial scaffolds”, Paolo Macchiarini told to the journalists.
Julia returned to Saint Petersburg to her family. Before leaving the hospital she thanked Professor Macchiarini and all team and sheared her plans: “I am going to spend more time with my child first, may be we’ll have a little trip, and then, in September, to start new studies. It’s a secret, but I’ll make a lot of changes in my life”.
Both Julia and Alexander told about their experience with two new candidates for transplantation who have now necessary observations at the Krasnodar Clinical Hospital.
The first bioartificial stem-cell based laryngo-tracheal transplantations were performed on June 19th and 21st at the Krasnodar Regional Hospital (Russia) by Paolo MACCHIARINI, professor of regenerative surgery at the Karolinska Institute (Sweden, Stockholm), and colleagues.
First bioartificial stem-cell based laryngo-tracheal transplantation
 The first bioartificial stem-cell based laryngo-tracheal transplantation was performed on June 19th at the Krasnodar Regional Hospital (Russia) by Paolo MACCHIARINI, professor of regenerative surgery at the Karolinska Institutet (Sweden, Stockholm), and collegues.
The first bioartificial stem-cell based laryngo-tracheal transplantation was performed on June 19th at the Krasnodar Regional Hospital (Russia) by Paolo MACCHIARINI, professor of regenerative surgery at the Karolinska Institutet (Sweden, Stockholm), and collegues.
Prof. Maccharini led an international team including Prof. Vladimir PORHANOV, head of oncological and thoracic department of Kuban State Medical University (Russia), Nanofiber Solutions (Ohio, USA) who produced the nanocomposite laryngo-tracheal scaffold and Harvard Bioscience (Boston, USA) who produced a specifically designed bioreactor used to seed the scaffold with the patient´s own stem cells. The cells were grown on the scaffold inside the bioreactor for two days before transplantation to the patient. Because the cells used to regenerate the trachea were the patient’s own, there has been no rejection of the transplant and the patient is not taking immunosuppressive drugs. This is also the first patient entering a clinical trial on regenerative medicine replacement, and is supported by a Megagrant of the Government of the Russian Federation, designed to invite the leading scientists worldwide to Russian universities..
 The patient, a 33 years old mother of one child from Saint-Petersburg suffered from a narrowing of the laryngo-tracheal junction for which she already had a failed previous surgery. Transplantation was the last resource for the patient to breath and speak normally and get a normal quality of life. Immediately after transplantation she was able to speak and breath normally, and has recovered completely.
The patient, a 33 years old mother of one child from Saint-Petersburg suffered from a narrowing of the laryngo-tracheal junction for which she already had a failed previous surgery. Transplantation was the last resource for the patient to breath and speak normally and get a normal quality of life. Immediately after transplantation she was able to speak and breath normally, and has recovered completely.
This transplantation program is supported by a Megagrant of the Russian Government to develop technologies in the field of the regenerative medicine. The main aim is the evaluation of the molecular mechanisms and underlying pathways of tissue-engineering and cell therapy for regenerating airways and lung .
Contacts:
Prof. Paolo Macchiarini
+46 760503213
Karolinska Institutet
For press:
Elena Kokurina
longevity.foundation@gmail.com
+7 985 1395088
Preliminary stage of training in Karolinska done
Young specialists from Kuban State Medical University, members of the grant research team, Elena Gubareva and Aleksandr Sotnichenko underwent the first stage of training in the Karolinska Institute (Sweden) in the department of regenerative medicine. They spent there the first two weeks 09.04.2012 – 23.04.2012.
Purpose of training: gaining of experience in laboratory of regenerative medicine, studying methods and ways of organs and tissues decellularization, seeding of bioartificial scaffolds for manufacturing of bioengineered trachea aimed at implementation of further work on the grant of the Government of the Russian Federation on direction “Molecular and cellular biology, biotechnology, regenerative medicine”.
Before training in the Karolinska the young researchers underwent training in Moscow and St. Petersburg at our partners – Human Stem Cells Institute and Institute of Cytology of Russian Academy of Sciences. There they mastered skills of work with cell cultures during a month in order to be able to proceed direct to research on the subject of the grant and be on the same level of grounding as their new colleagues.
The next stage of training will begin on the 25th of June and last for 3 months. After that E.Gubareva and A.Sotnichenko will work in their own laboratory, in Kuban Medical University.
V Annual International Symposium “Topical issues of gene and cellular technologies”
On May 28, 2012 Professor Paolo Macchiarini will participate in the V Annual International Symposium “Topical issues of gene and cellular technologies” in Moscow with the presentation: "Lessons learned from natural and synthetic bioengineered tracheal transplants and implications for future organs"
Here you can find the program of the conference and to register
International video conference - important step for transplantation
On February 16, 2012 the first international video conference on regenerative medicine headed by the leading scientist professor Paolo Macchiarini took place in Clinical Regional Hospital after prof. Ochapovsky within frames of the grant money of the Government of the Russian Federation. Russian and foreign hospitals took part in this conference: Stokholm – Huston – Krasnodar – Florence – Moscow. Possibilities of bioengineered tracheal transplantation for patients with diseases of upper airways were discussed during this online conference. Karoliska Institute (Sweden, Stockholm) represented one patient. Specialists from National Research Centre of Surgery named after B.V. Petrovsky, Russian Academy of Medical Sciences, Moscow, represented case of the patient who had cadaveric tracheal transplant. Surgeons of University Hospital Careggi (Florence, Italy) also represented one patient; and surgeons of Texas University (USA) offered two candidates, including one child.
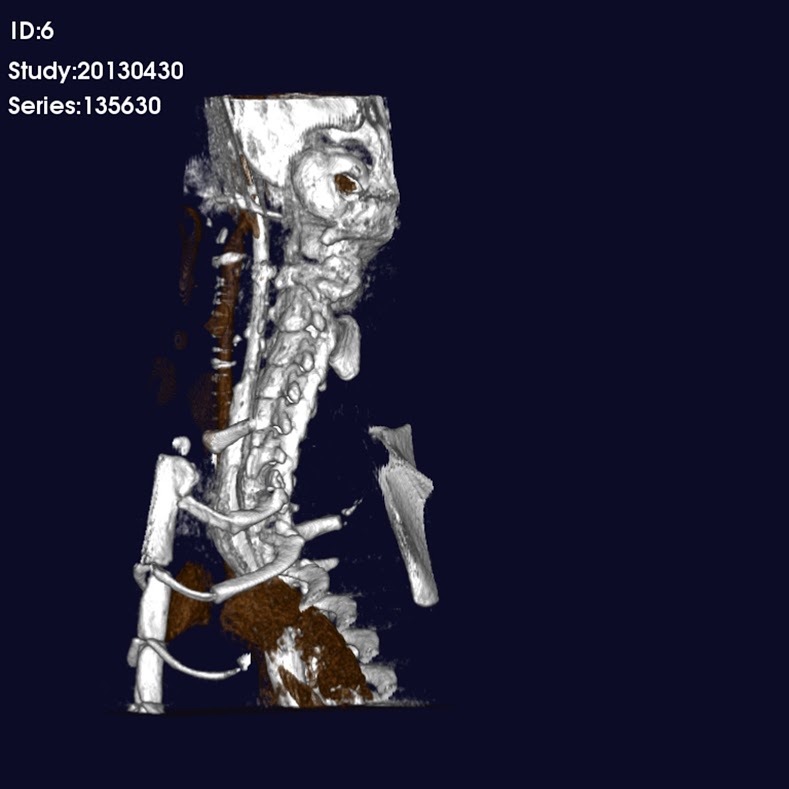
Thoracic surgeon, Deputy Head Doctor of Clinical Regional Hospital ¹1 I.S. Polyakov who is responsible for preparing working with the patients to the upcoming transplantation reported results of instrumental evaluations: CT and bronchoscopy of two candidates. Candidates were discussed by leading specialists of participating countries. Everybody could share his opinion about treatment process and case management.
Several transplantations of nanocomposite trachea seeded by autologous mesenchymal cells of patient are planned within this project. For the present moment preparing work is under way.
 Main page
Main page